My Baby is Breech: My Experience Getting an Unmedicated ECV
Did you know only 3-4% of full-term (37-weeks) pregnancies are breech? I didn’t. It wasn’t until I was further along into my second pregnancy that I started to research this more and what it means to have a breech baby.
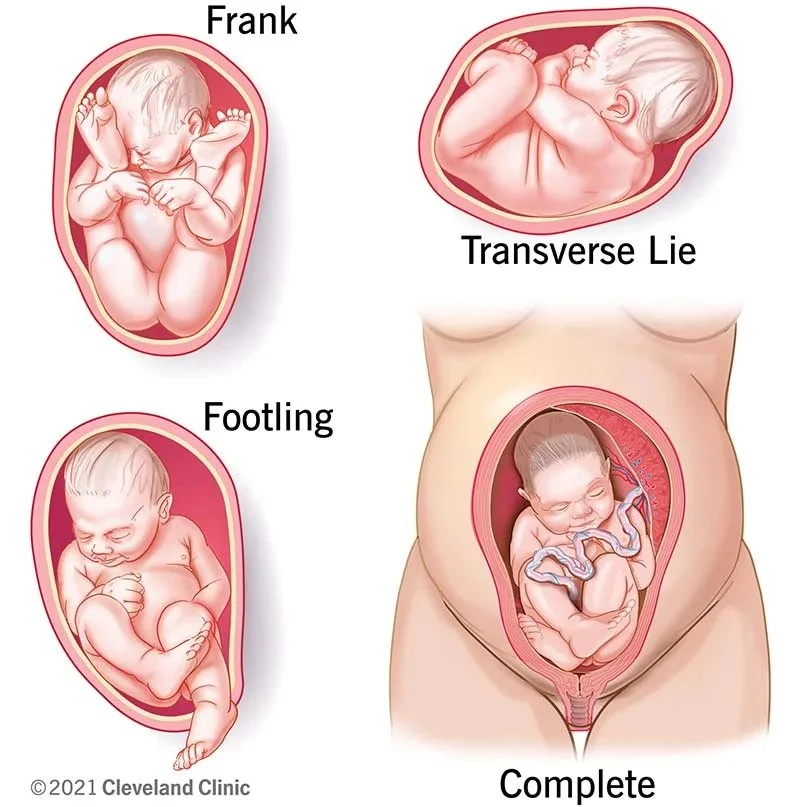
If you’re not familiar with the different ways a baby could be positioned in the uterus, a breech baby is when your baby is not in a head down position near your cervix, which is the ideal position for a vaginal delivery.
There are different types of breech positions including:
Complete: Both of the baby's knees are bent and their feet and bottom are closest to the birth canal.
Incomplete: Only one of the baby's knees is bent and their foot and bottom are closest to the birth canal.
Frank: When the baby's legs are folded flat up against their head and their bottom is closest to the birth canal.
Footling: Where one or both feet are presenting in the birth canal.
Transverse: Where the baby's head is on one side of the mother's body and the feet are on the other.
Most doctors will not recommend or perform vaginal deliveries on babies in the breech position. According to Parents.com, “When babies are in a breech position, several potential delivery complications emerge. For starters, their feet or bottom may tangle with the umbilical cord, causing issues such as umbilical cord prolapse. Their body may also emerge from the cervix before it's fully dilated, and the head (the biggest part of the baby) may get stuck in the birth canal.”
So, if my baby is in a breech position, what are my options? It varies. It’s based on your medical history, the health of your pregnancy, number of pregnancies or babies you’ve had, location of the placenta, your birth plan and more. If you’re scheduled for a cesarean (c-section), then having a breech baby most likely won’t be a concern for your doctor.
If your birth plan does include having a vaginal delivery, then you have a couple of options to consider. You can try different exercises or assistance to help get your baby to naturally flip on its own, schedule an External Cephalic Version (also known as an ECV or version) or find a doctor who’d be willing to work with you to birth your baby in the breech position.
Although delivering in a breech position is not recommended by most doctors, it’s still an option you can explore and have a conversation about based on what you feel is right for you and your baby. Later, I’ll explain what natural options you can consider, but for now I’ll explain more about the details of getting an ECV, and what you can expect based on my experience with getting one.
Typically, this procedure is done at 37-weeks, where two doctors apply pressure on the outside of your stomach to lift the baby’s head and butt from being in a head up position to a head down position near your cervix. If the idea of this procedure has you curling your toes, you’re not alone. There were so many thoughts running through my head when I first heard of this procedure, like:
Is an ECV painful?
If it is, what does pain management look like?
Is it safe for the baby?
How many women typically get ECVs?
What is the success rate of getting an ECV?
What happens if the ECV isn’t successful?
How long is the procedure?
Where will the procedure be performed at?
Are there any other options to avoid an ECV?
The list went on and on. Even with all the questions I had circling in my head, no matter what the answers were and if I liked them or not, the safety of our baby was our top priority. What made this decision hard was that it was difficult to find close friends or family members who had experienced having a breech pregnancy and then also having an ECV.
In short, I was able to have a successful unmedicated ECV, and here’s what made me an ideal candidate:
I wanted a vaginal delivery,
This was my second baby,
Baby was in a complete breech position,
The placenta was in the middle of my uterus and posterior, and
My pregnancy was low risk with zero complications.
With that, there can be other factors that can help determine if an ECV is the right option for you, so make sure to have a thorough conversation with your doctor about it.
What’s the success rate of an ECV? According to the data, the success rate of this procedure is reported to be 58% and that’s because each woman, pregnancy, and how one manages applied pressure or pain during the procedure can vary. There are also ways you can increase your odds of it becoming a success. For instance, getting an epidural can increase your odds by 23% versus not getting one.
Is it really necessary to get an epidural if it’s a short procedure? As far as timing, most ECVs are performed between 5-10 minutes. The time it takes to complete the procedure also depends on how many attempts your OB and the assisting physician will perform it in order to re-position the baby to get them heads down. This is important because there are several outcomes of what could happen and why having pain management can play into it.
For instance:
Baby flips, which is the best-case scenario, and your doctor performs a successful ECV, so you’re able to wait for a spontaneous delivery to happen.
Baby does not flip, and you have to be scheduled for a c-section at a later date.*
Baby becomes distressed and the heart rate falls under 100 beats per minute (bpm) and then you are rushed to have an emergency c-section performed.
Baby (flips or does not flip) becomes distressed after the procedure and during your 45-minute to hour wait time, your doctor recommends that a c-section be performed that day for the safety of you and your baby.
*Remember, you have the decision and power to decide if you want to deliver your baby breech or not.
All these outcomes carry a different weight to them, as it relates to your pain management, which is why it’s important to talk through all your options with your doctor, partner, hospital anesthesiologist, and midwife or doula (if you have one), so you can make the best and most informed decision for you.
Should my ECV be medicated or unmedicated? This was by far the hardest decision I had to make, and I didn’t have a clear answer until 15 minutes before the procedure. To be clear, it also wasn’t a matter of me being indecisive. It truly came down to new information being shared with me up to the day.
With medication, you can either get an epidural or spinal tap to assist with pain management. It’s still a bit unclear to me about the differences, but make sure you understand if your hospital offers one or the other, or both. My hospital only offered an epidural for this procedure and didn’t have a real reason for why spinal taps weren’t offered.
To slightly explain the differences between the two, a spinal tap numbs you from the chest down whereas an epidural numbs you from the stomach down. Each option would require you to stay in the hospital longer (with the possibility of an overnight stay) than if you did the procedure without one.
The benefit of getting an epidural or spinal tap is that it allows you to relax more during the procedure, and it has a greater success rate of the baby flipping versus doing the procedure without.
It also helps to have an epidural in the small chance that an emergency c-section does have to be performed, and you can be fully awake for the delivery of your baby. If you don’t have an epidural and you’re required to get an emergency c-section then you’d have to be put down with general anesthesia, which means you’d have to wait to wake up from the procedure to meet your baby. Again, this can be lot to process, but it’s important to consider the probabilities of each of these scenarios happening and what would work best for you.
Last, speak with your hospital’s anesthesiologist (preferably days before the procedure rather than the day of). For me, this was helpful because mine informed me that most of her ECV patients who received an epidural were ultimately disappointed because it did not eliminate all pain from the procedure. For me, if it didn’t eliminate all pain, then it wasn’t worth it especially if I’d have to wait hours for it to wear off.
So, how did I end up in this position? Pun intended. I’ll never forget the day, where my husband, doula, and I were told by my doctor, “Your baby is breech,” at my 32-week appointment. “But there’s still plenty of time for her to flip, so if she hasn’t turned heads down by then, we’ll discuss additional options of what we would need to do next.”
She said all this with no concern or worry in her voice, so I didn’t worry about it either. Her confidence left me feeling reassured that at my next appointment (which was at 36-weeks), our baby girl would be heads down and I’d be mentally preparing for a spontaneous labor and delivery.
When I got home that night, I did a bit more research which led me down a rabbit hole of, “Well…what happens if she doesn’t flip?” and that’s when I started to panic. This was based on all the information I stumbled across along with the mid-range percentages of success. Also, why was my doctor so calm and confident about it?
It felt like my options were limited as well as time sensitive, so I started looking into any and everything on ways to get this baby to flip. I tried it all: Spinning Babies, acupuncture, moxibustion, cat cow positions, balancing on a yoga ball, and laying on an ironing board upside down multiple times a day. If this sounds like it a lot, I’d like to confirm that it was, but I was willing to try any and everything to avoid getting an ECV.
Why did I choose to have a medicated ECV as my first decision? The data varied along with the stories that were shared with me. I had one friend who told me getting an ECV unmedicated was extremely painful and if she could have done an epidural she would have but based on her medical history she couldn’t get one. She also confirmed not having a successful unmedicated ECV and later had to schedule a c-section.
I had another friend tell me she had an ECV unmedicated and it was more painful than birth, which definitely scared me a bit and it ultimately resulted with her getting a scheduled c-section at a later date because the attempt she tried had failed.
The last experience I heard was from a co-worker, who said she did a spinal tap, and her experience was a success, and she did not feel an ounce of pain from her chest down. She was able to have a vaginal delivery which led me to believe that getting an epidural or some kind of pain medication would increase my odds of it being a success for me.
Also, the research I had come across also confirmed there was a greater chance of success if pain management was included. When I got to my 36-week appointment, we checked the positioning of my baby’s head and there she was… still in a breech position.
My ECV was scheduled for that following Friday. I was hoping she would turn before then, so we could cancel it, but as each day drew closer and closer I didn’t feel any major shifts which led me to believe this procedure was happening and I needed to get mentally prepared for it.
The day prior, I went to the hospital to get my blood drawn, so they would have my blood type nearby just in case of an emergency c-section, and it started to settle in that there was a slight possibility that she could be born the day of the procedure. I stopped thinking that the possibility of a c-section was small because having a breech baby was also small.
I started to embrace my reality, and spoke with my husband, doula, and my doula’s clinical team on what I wanted to do. I was still struggling on whether I wanted to get an epidural versus not getting one based on my doctor’s confidence of doing this procedure without one.
Unfortunately, I didn’t get a chance to talk to my doctor about it until the day of, but I felt good that getting an epidural was the best option for me. It wasn’t an easy decision to make because epidurals are expensive, and I knew I wanted to have an epidural for labor and delivery. Personally, I felt like it was unnecessary exposure, but for the best chance of increasing my odds of a successful flip, it felt like this would be the best way to go if I wanted a vaginal delivery.
The night before the procedure, we both packed our hospital bags, spent a little extra time with our first born, and mentally started to prepare for what could happen the next day, which could have been welcoming our second born to the world. It was a reality we were both settling in to and we had both our parents on standby along with our closest friends.
The morning of the procedure, my husband and I woke up speaking positive affirmations and prayers into the day and dropped off our first born at daycare. Unfortunately, I wasn’t able to eat anything because I was required to fast eight hours prior to it, but I felt good all things considered.
Our expected check-in time was at 9:30 a.m. and then the procedure wasn’t scheduled until 11:30 a.m. It was a rainy morning, and we were hopeful that the day would be uneventful, and we’d be back at home in the late afternoon. When we arrived, my husband and I checked into labor and delivery, and it all started to feel a bit too familiar.
My doula was expected to arrive within the hour, so we were directed back to our room, where I changed into my hospital gown and tried to get as comfortable as I could. It was then I asked my nurse if she could inform my doctor that I wanted an epidural. She asked if my doctor was aware of my decision, which I then told her I hadn’t, and it was a last-minute decision.
Not too long after, she told me she was able to speak with my doctor who advised against getting the epidural, but she did say my doctor would honor my decision if that’s what I wanted. At this point, I had decision paralysis. I was anxious, uncertain, and overwhelmed. My doula was on Facetime, the hospital midwife was performing an ultrasound on me, and the nurse was asking me what I wanted to do and if speaking to the hospital anesthesiologist would be helpful.
In this moment, I went silent. I knew a decision would be needed, but I wasn’t confident at all. I started to feel powerless, which was the exact same feeling of what I felt with my first. What made it even worse was the nurse who was trying to set-up my IV failed to get the needle into my vein twice, which shot my anxiety through the roof.
Thankfully, after I spoke with the hospital anesthesiologist, I had all the information I needed to make an informed decision. I was going to do the ECV without an epidural. Here was my thought process:
I never really wanted to get two epidurals within two weeks of each other. I truly felt like the unnecessary exposure was secretly bothering me, so doing it unmedicated aligned with my original birth plan.
Although an epidural increases the odds of an ECV being a success, I didn’t feel confident that it would eliminate all the pain of the procedure, which to me defeated the purpose of getting one.
Epidurals are expensive and I really didn’t want to have to pay for two of them because I knew I wanted to have one for labor and delivery.
I didn’t want to do an overnight stay in the hospital (especially if the procedure wasn’t a success), and the total time of the procedure is only a few minutes.
My doctor’s confidence level. She’s NEVER performed an ECV that’s led to an emergency c-section. That’s a good track record in my book, plus she said she was REALLY good at them.
Last, if the ECV was too painful for me to handle, I could tell them to stop. I had the power, and this led me to feel so much more confident.
Even though it took me longer than I would have wanted to make this decision, I felt empowered and supported with how I wanted to move forward. After I made my decision, my nurse gave me a terbutaline shot in the back of my right arm, which helped relax the muscles in my uterus to help prevent contractions.
Instantly, I felt like I had several shots of expresso. The medication I took is known to increase your heart rate, which allows the doctors and staff to know that it’s working. From there, my husband started playing music, which made me feel even more relaxed. I started to focus on my breathing and was finally ready to go.
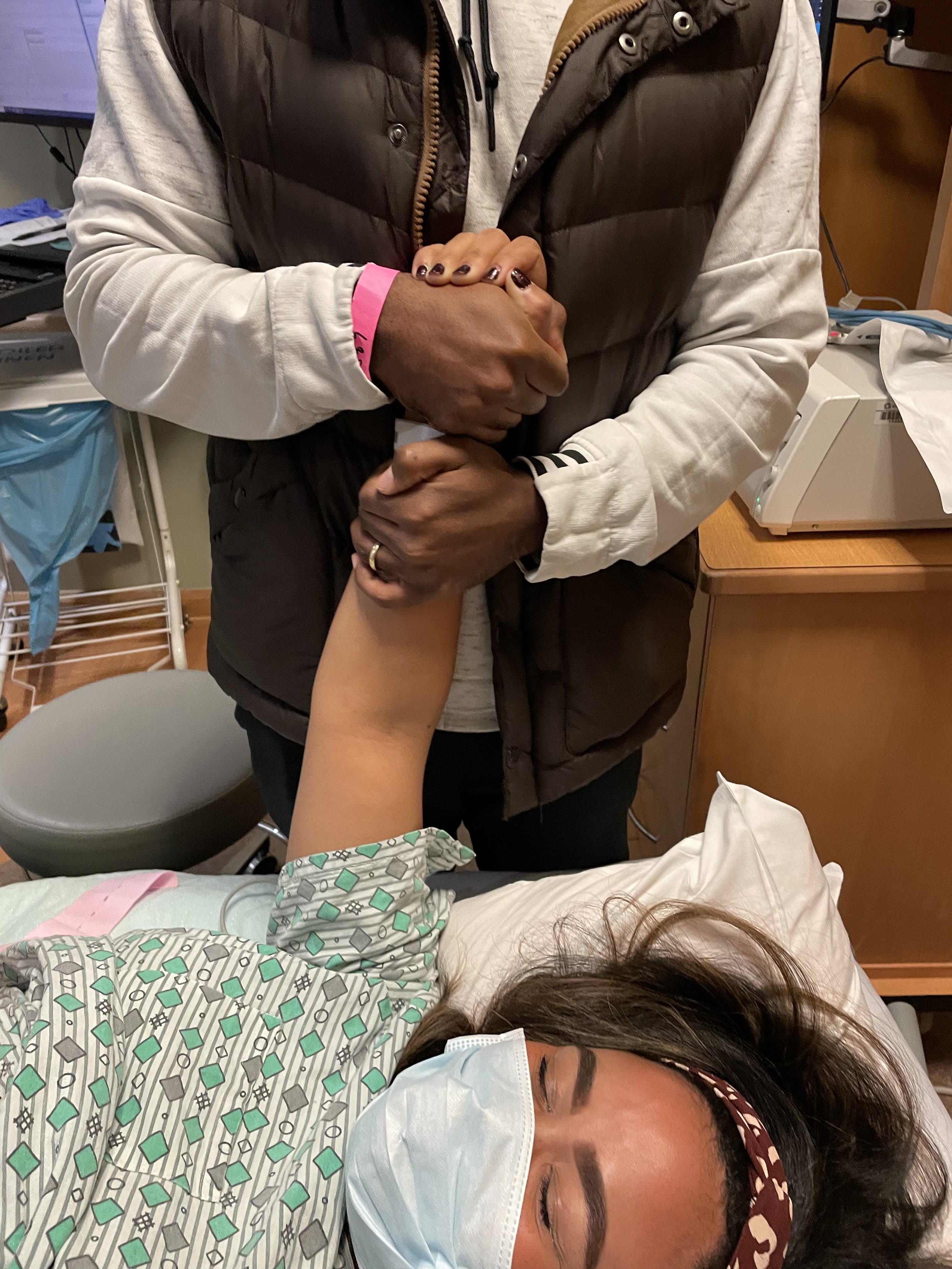
It was almost game time and soon enough my doula, doctor and the supporting physician of the procedure came into the room. Once more, my doctor explained to me how the procedure would start and introduced me to the supporting physician. Soon, they positioned themselves at the lower half of my body, while my husband was on my top right and my doula was on my left.
From there, my doctor confirmed once more that baby was in the breech position by ultrasound and then she started to gently feel around stomach looking to identify the baby’s head and butt. As she navigated how she was going to re-position the baby, the song “Lift Off” by Jay Z and Kanye West featuring Beyonce started playing.
Without a countdown, my doctor started to apply pressure and began pushing the baby’s body toward the doctor on the other side of me which helped lower the anticipation and build-up of it. I was laid all the way down on my back and was looking at nothing but the fluorescent lights in the ceiling while also listening to the music.
My husband was holding my hand saying, “You got this” and my doula was telling me to “Focus on the music.” I took several deep breaths and did exactly what they said. With just a few moments of intense pressure and slight pain that forced me to clench my fists and curl my toes, my doctor then says, “She’s down.” She turned the ultrasound machine toward me, and all I could do was cry. I looked at both my husband and doula and felt so much pride in what just happened.
All the built-up anxiety and decision-making was over. She was finally in the position she needed to be in, so we could have a vaginal delivery. I could finally reclaim my time in a hospital that gave me such beauty with my first born, but also so much pain. I was so grateful I could go home that day and share the good news with family and friends.
Her heart rate was steady, and now all we had to do was monitor it for the next hour, so we could be cleared to go home. Through all of it, if I had to make the same decision again, I would. I’d listen to all the stories, look up all the research, and try all the different exercises to get her to flip. I feel so much stronger knowing my body allowed me to have this procedure.
For anyone reading this that’s currently pregnant and contemplating an ECV, whether medicated or unmedicated, please feel free to reach out to me. I’m sharing my story and experience for you, so you can feel just as empowered and informed as I did. I’m so thankful for those who helped me along the way.
When you think you only have so much left to give, tell yourself to give just a little bit more. We always tend underestimate how far we can really go. I want you to surprise yourself. You’re so much stronger than you think.